By Charlotte Webster-
The chair of the council of the British Medical Association has today claimed that the NHS is “riddled with racism” following the findings of a survey into the experiences of doctors.
The survey of 2,000 doctors found that at an estimated 60% of those who had been subject to abuse said it had negatively impacted their wellbeing, including causing depression and anxiety.
At least 75 per cent of ethnic minority doctors experienced racism more than once in the past two years, and 17.4 per cent claimed to have experienced regular racism at work.
Interim findings from the union’s ‘Racism in Medicine’ survey showed that just over 90% of black and Asian respondents, 73% of mixed and 64% of white respondents, said racism in the medical profession is an issue, while 20% of consultants who had experienced racism reported racist behaviour from patients.
The study also found a fifth of doctors had either considered leaving (13.8%) or left their job (5.6%) within the past two years due to race discrimination.
Despite high levels of racism being reported by doctors, more than 71% of those who had suffered racism chose not to report it to anyone due to ‘a lack of confidence that the incident would be addressed’ ,or ‘a fear that they would be labelled ‘troublemakers’ – with six in 10 saying that reporting a racist incident had a negative impact.
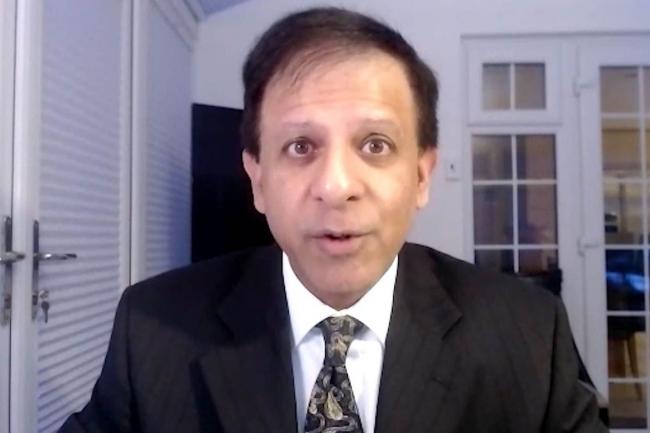
BMA chair Dr Chaand Nagpaul condemned ‘unacceptable levels of racism within the NHS’ following the results and has warned that it is ‘undermining the NHS’ ability to bring out the best in its workforce’. He has also accused decision makers of ‘having their heads in the sand’ over the issue.
The results of the BMA survey come just two weeks after the CQC admitted that GP practices led by doctors from ethnic minorities may be ‘disadvantaged’ by its regulation process, adding that ethnic minority-led practices ‘are often not operating on a level playing field’.
A total of 59.7% of Asian doctors, 57.3% of black doctors, 45.1%, of mixed ethnicity doctors and 36.3% of white non-British respondents saw racism as a barrier to career progression compared to just 4.2% of white British respondents, the survey found.
Doctor abuse
The BMA also shared comments from doctors involved in the survey that highlight the abuse they have suffered at work from either patients or colleagues. One consultant of Indian background working in the NHS said: ‘I was not taken seriously. Emails were ignored. I suffered work related stress and hypertension. I think of leaving this job every day.’
Another junior doctor of ‘mixed-other’ ethnic background said she was called a ‘headscarf b**ch’ by a patient. Another junior doctor said: ‘Working in A&E was a nightmare. Continued racist behaviour from patients and their relatives. Due to this, I have decided not to pursue a career in emergency medicine.’
Last year the BMA launched its first national member forum for black, Asian and minority ethnic (BAME) doctors and medical students. Dr Nagpaul argued the government had to step up and address issues of racism. He said: ‘The results from this survey, though interim, show unacceptable levels of racism within the NHS which cannot be ignored.
‘Doctors from ethnic minority backgrounds and those who qualified outside the UK, but are registered to practice here, want to focus on caring for patients, without the burden of abuse that comes from demoralizing and often debilitating experiences of racism in the workplace.
One missing element from the report was how much of the racism experienced came from other Nhs employees, and how much came from patients.
Sewell report
‘The findings highlight the negative impact that racist experiences have on doctor retention, wellbeing, and career progression – an indisputable rebuttal to the government’s claims in its Sewell report that the NHS is a success story for ethnic minority doctors.
‘Portraying the NHS as a success purely because of the numbers of staff from ethnic minority backgrounds employed within the service, shows little acknowledgement of the racist incidents that these staff members deal with on a regular basis.’
The Sewell report published last year found that the UK was not yet ‘a post-racial society which has completed the long journey to equality of opportunity’. It concluded, however, that ‘most of the disparities we examined, which some attribute to racial discrimination, often do not have their origins in racism’.
The paper was criticzsed by the BMA, which called it a ‘missed opportunity’ and said that evidence of structural racism in the NHS was ‘enormous’ and significantly affected outcomes and life chances for ethnic minority healthcare workers.
Dr Nagpaul added: ‘These experiences of racism are clearly undermining the NHS’ ability to bring out the best in its workforce and there is no doubt that this will be having a knock-on effect on patient services…It’s high time the conversation on race equality in the medical profession changes – reflects NHS staff’s lived experiences and seeks solutions.
‘Employers and the government have a duty of care to address the concerns of those who work within the health service. Decision-makers must get their heads out of the sand and act now.’
The BMA will publish its full ‘Anti-Racism in Medicine’ report with ‘a series of recommendations’ this Spring, and will outline the causes of race inequality in the health service.
NHS medical director of primary care Dr Nikki Kanani said: ‘There is never an excuse for racism or any form of discrimination and it should not be tolerated by anyone, including our hard-working and dedicated NHS staff.
‘While our latest equality report shows that we have made progress in some areas of the NHS, it is completely unacceptable for anyone to experience racism, discrimination or prejudice at work and NHS organizations should continue to take a zero-tolerance approach to all and any form of discrimination.’
Speaking to the BBC BMA council chair Dr Chaand Nagpaul said: “This is about a moral right for anyone who works for the NHS to be treated fairly.”
The NHS’s medical director of primary care, Dr Nikki Kanani, responded by telling the broadcaster that racism and discrimination of any kind “should not be tolerated by anyone”.
“While our latest equality report [in 2020] shows that we have made progress in some areas of the NHS, it is completely unacceptable for anyone to experience racism, discrimination or prejudice at work, and NHS organizations should continue to take a zero-tolerance approach to all and any form of discrimination,” she said.
Almost 20 per cent said they considered leaving their job or had left their job in the past two years because of racism.
Nearly 60 per cent said racism at work had impacted their mental health and wellbeing, and 20 per cent said they experienced racism from patients.|